| Journal of Current Surgery, ISSN 1927-1298 print, 1927-1301 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Curr Surg and Elmer Press Inc |
| Journal website https://jcs.elmerpub.com |
Case Report
Volume 000, Number 000, April 2025, pages 000-000
Chronic Non-Infected Branchial Cleft Cyst With Jugular Vein Displacement: Diagnostic and Surgical Challenges in a Rare Neck Mass
Muhammad Uzaira , Husam Jamilb, c
aENT Department, POF Hospital, Wah Cantt, Rawalpindi, Pakistan
bST7 Acute Medicine, Yorkshire and Humber Deanery, Leeds, UK
cCorresponding Author: Husam Jamil, ST7 Acute Medicine, Yorkshire and Humber Deanery, Leeds, UK
Manuscript submitted January 4, 2025, accepted March 14, 2025, published online April 5, 2025
Short title: Chronic BCC With Jugular Vein Displacement
doi: https://doi.org/10.14740/jcs1004
| Abstract | ▴Top |
Branchial cleft anomalies are rare embryonic developmental abnormalities. We discuss a case of a 23-year-old female, who presented with a progressively enlarged swelling on the right side of her neck, which had been present since 2016 (8 years ago). Initially asymptomatic, the swelling progressively transformed, triggering intermittent pain during sore throat, and specific activities like loud speaking or long journeys. Multiple aspiration procedures offered temporary relief but failed to resolve the underlying pathology. The diagnostic challenge was profound, as it involved a rare condition mimicking more prevalent regional pathologies, such as tuberculosis and lymphadenopathy, particularly in Pakistan. Ultrasound, computed tomography (CT) scan and magnetic resonance imaging (MRI) meticulously mapped the lesion’s intricate anatomical relationships. These diagnostic modalities strongly suggested a second branchial cleft cyst, subsequently confirmed through histopathological examination. Surgical intervention involved complete cyst excision performed under general anesthesia. Microscopic analysis revealed a unilocular cyst with characteristic stratified squamous epithelial lining and associated lymphoid tissue. Critically, no malignant transformations were detected, with accompanying lymph nodes demonstrating benign reactive changes. This case is unique due to jugular vein displacement due to branchial cyst and the absence of infection over an extended period, from 2016 to 2024, despite the cyst’s tendency for infection as reported in the literature. It highlights the importance of early diagnosis, advanced imaging, and complete surgical excision to achieve favorable outcomes. Learning points include recognizing branchial cleft cysts in the differential diagnosis of lateral neck masses, the essential role of imaging in diagnosis and surgical planning, and the significance of histopathology in confirming the benign nature of such anomalies.
Keywords: Branchial cleft cyst; Neck swelling; Second branchial cleft cyst; Neck mass
| Introduction | ▴Top |
Branchial cleft anomalies (BCAs) include branchial fistulas, sinuses, and cysts. These are rare congenital developmental abnormalities during embryogenesis [1]. The branchial apparatus consists of arches, clefts, and pouches. The branchial apparatus is very important in head and neck development. Initially, there are six branchial arches but the fifth is rudimentary and eventually disappears. During development, the second branchial arch grows downward, overgrowing the third and fourth clefts to form a temporary cavity called the cervical sinus. Normally, this sinus is obliterated by the seventh week of gestation. Failure of this process results in branchial anomalies [2]. Branchial cleft cysts (BCCs) are the most common type of BCA and the second most frequent congenital anomaly of the head and neck, following thyroglossal duct cysts [3]. BCCs are typically diagnosed in children and young adults, but they can also present later in life [4].
BCAs are classified into four types: first, second, third, and fourth. Second BCAs are the most common, which accounts for approximately 90% of cases [4, 5]. Among BCAs, cysts are the most common manifestation, followed by sinuses and fistulas [6]. Although typically benign, these anomalies can cause significant morbidity due to infection, abscess formation, or misdiagnosis as other neck masses.
Second BCCs are classified into four types by Bailey: 1) Type I is located in the periparotid region, potentially extending toward the external auditory canal. It may involve the facial nerve, complicating surgical removal. 2) Type II, the most common type, is located in the submandibular region, anterior to the sternocleidomastoid (SCM) muscle. It may extend between the internal and external carotid arteries, typically presenting as a neck mass. 3) Type III extends deep to the carotid arteries and may involve the lateral pharyngeal wall and parapharyngeal space. This rare type is challenging to diagnose due to its complex presentation. 4) Type IV, the rarest form, is located deep and medially in the parapharyngeal space. It often lacks a visible neck mass, complicating diagnosis [3, 6].
In this case report, we present a young female with second BCC having unique features. BCCs are prone to infection, but this is a unique case as it remained non-infected for such a long period from 2016 till 2024. What was more unusual was that the jugular vein was displaced and effaced by the cyst. This feature has not yet been reported in the literature. This is a peculiar finding which underlines that such lesions can potentially interfere with the vascular anatomy.
| Case Report | ▴Top |
Investigations
A 23-year-old female patient presented with complaints of a progressively enlarged swelling located on the right side of her neck since 2016. Initially, there was no pain but increasingly started to cause pain during episodes of sore throat or long journeys or after speaking out loud. It was not linked with dysphagia or dyspnea at all. There was no significant past medical history and family history. She has no family history of tuberculosis or any other chronic conditions; otherwise, psychosocial background is insignificant.
On physical examination, a non-tender, soft, and compressible mass was noted located immediately anterior to the SCM muscle on the right side of the neck (Fig. 1).
 Click for large image | Figure 1. Neck swelling of the patient. |
In 2016, aspiration of the swelling was performed, and the cytology report indicated the presence of superficial squamous cells. Her general practitioner (GP) prescribed antibiotics, and the mass persisted. She had two more aspirations of turbid fluid from the cyst, which reduced the swelling temporarily, but it subsequently increased in size again. The culture and sensitivity reports of the yellowish fluid were negative each time.
In 2021, it was considered as a case of lymphadenopathy, so a cervical lymph node biopsy was performed to explore this further. Biopsy findings showed reactive lymphoid follicular hyperplasia along with fragments of squamous-lined tissue consistent with a lymphoepithelial cyst. There were no granulomas or malignancy, but the diagnosis remained inconclusive.
Ultrasonographic examination of second BCCs typically reveals a well-circumscribed cyst. However, there can be some variations in ultrasonographic appearance due to secondary infection, internal septa, or cellular debris, which may result in a pseudosolid or heterogeneous appearance [7].
Magnetic resonance imaging (MRI) findings revealed a cystic lesion in the right submandibular region with inferomedial extension into the posterior cervical space. The lesion measured 3.6 × 3.2 × 1.5 cm, supporting the possibility of a cystic lesion such as a BCC.
Notably, computed tomography (CT) scan findings indicate that the cyst displaced the jugular vein posteromedially, causing effacement in this segment, although no significant vascular compromise was observed (Fig. 2). There was no cervical lymphadenopathy, and the surrounding structures were normal. The tuberculosis (TB) Gene Expert test was also negative, which ruled out TB from differentials.
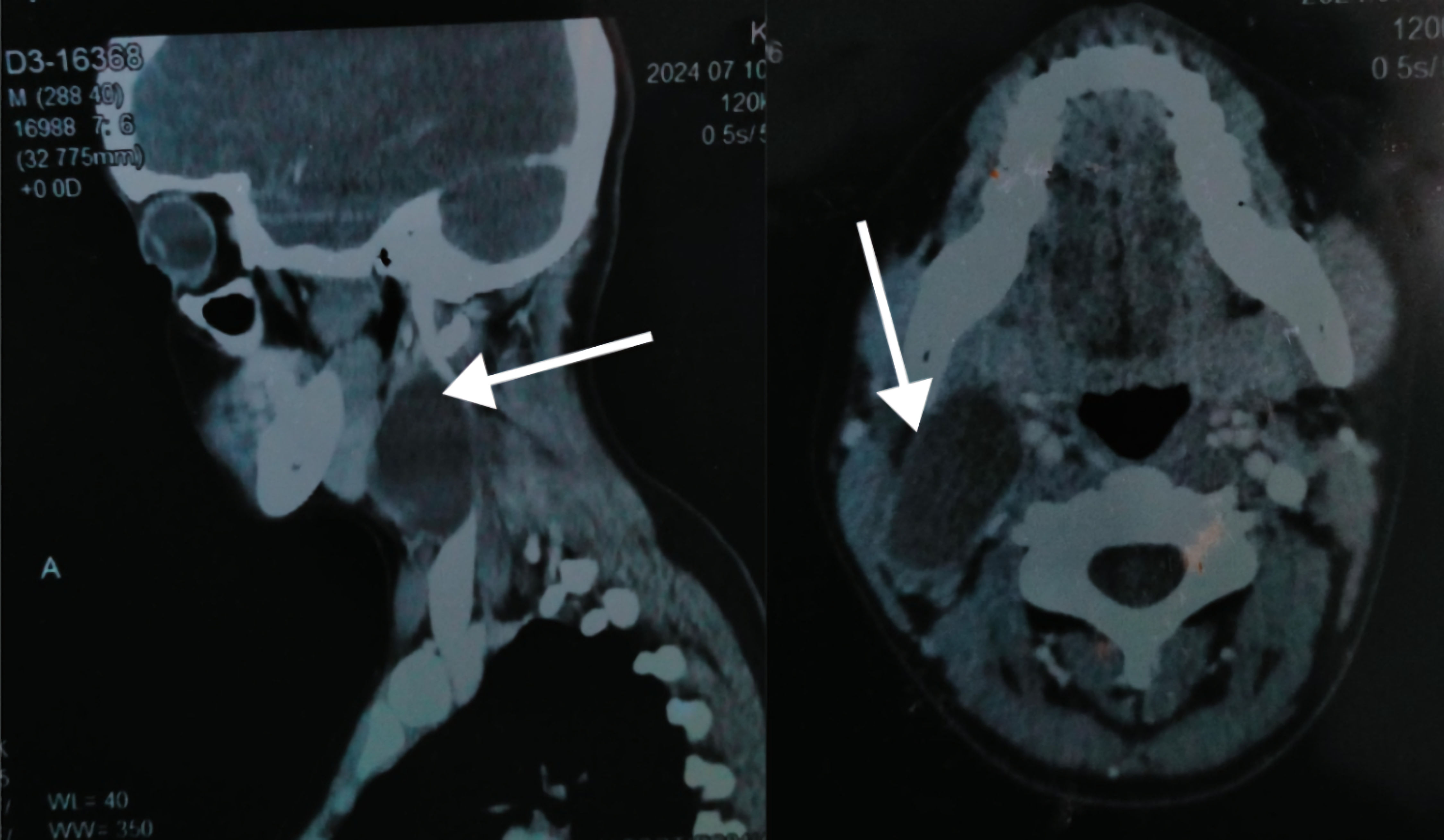 Click for large image | Figure 2. Computed tomography (CT) scan, with arrows indicating the branchial cleft cyst. |
Diagnosis
The diagnosis of the second BCC was based on clinical findings, ultrasound, MRI, and CT scan. Cytology was suggestive of squamous cells, whereas MRI and CT scans revealed characteristic cystic features.
The differential diagnosis includes: 1) BCC (most likely, based on imaging and cytology); 2) Lymphangioma (a congenital lymphatic malformation, usually more irregular in shape); 3) Tuberculous abscess (unlikely, as the test for TB Gene Expert test is negative, and there is no granuloma formation or systemic illness).
Fine needle aspiration cytology has diagnostic sensitivity of 100%, a positive predictive value of 100%, and an accuracy rate of 100% in diagnosing a second BCC [8].
Treatment
The treatment of choice for the second branchial cleft anomaly is complete surgical excision [1, 9]. This surgery was done under general anesthesia in August 2024. A 4 cm transverse cervical incision was made along the anterior border of the sternocleidomastoid muscle to gain access for the meticulous excision of the cyst. The cyst was systematically separated from the surrounding tissues to reduce the risk of injury to adjacent anatomical structures.
The drainage tube was placed in the surgical site to avoid seroma development. After the surgery, antibiotics were administered to avoid infection and analgesics to fight pain. The patient was discharged on the third day of postoperative care, with follow-up.
Follow-up and outcomes
The patient complained of mild pain and swelling that were gradually reduced. At the 2-week follow-up, the surgical wound was clean without any sign of infection or any complication. The sutures were then removed. Two months post-surgery, the patient had no complaints. Healing was normal, and no signs of recurrence were found. The patient was satisfied with the treatment outcome.
| Discussion | ▴Top |
BCCs are congenital anomalies of the branchial apparatus, and they represent approximately 90% of all such anomalies in the world [4, 5]. The global incidence of BCCs is not known yet; however, their number is rarely documented in Pakistani literature due to a lower index of suspicion and clinical features often mimicking commonly seen conditions like tuberculosis and lymphadenopathy.
During embryonic development, the second branchial arch descends and covers the third and fourth arches, which causes the formation of a transient space called the cervical sinus. If this sinus fails to undergo obliteration by the seventh week of gestation, it causes the persistence of epithelial remnants, which may eventually develop into cysts, sinuses, or fistulas [2]. This developmental anomaly explains the occurrence of BCCs and their potential to remain asymptomatic for extended periods, as in the case presented here.
BCCs do have a nonspecific presentation; they often mimic the appearance of common conditions like lymphadenopathy or tuberculosis. Pakistan is estimated to be the sixth country in the world regarding TB burden, with almost 1.5 million people out of a population of 210 million affected by the diseases [10]. This high prevalence significantly influences the approach to diagnosing in chronic neck swellings, where tuberculous lymphadenitis is commonly the first diagnosis. Most likely congenital anomalies, such as BCCs, are then ignored, and the diagnosis is either delayed, or anti-tuberculosis treatment is unnecessarily given. This case emphasizes the importance of maintaining a wide differential diagnosis in the areas affected by the TB endemic for timely and proper surgical management.
In this case, for 8 years, the swelling went on before any proper and definite diagnosis was attained via advanced imaging studies. MRI and CT scans have provided valuable information regarding the characteristics of the cyst and its relation to the adjacent structures like the jugular vein, which was displaced and effaced by the lesion. However, there was no evidence of vascular compromise. Detailed imaging, therefore, underscores its importance in the preoperative plan.
Histopathological analysis confirmed the diagnosis, revealing a unilocular cyst lined with stratified squamous epithelium and lymphoid tissue with germinal centers. These findings are consistent with benign BCCs described in the literature.
Complete surgical removal is the cornerstone of the treatment because incomplete resection carries an increased risk of recurrence [11, 12]. The literature also reveals that the recurrence rate is 3% following primary excision, which increases to 14-22% after partial excision or infection [13]. However, this risk may be prevented by managing any active infections preoperatively with antibiotics [4].
This case had limitations. There is a relative lack of epidemiological data on BCCs in Pakistan, and limited follow-up studies on such patients. Further research is essential to improve the understanding of this rare anomaly and document long-term patient outcomes.
Learning points
BCCs are rare congenital anomalies which present as lateral neck masses. These cysts may often mimic more common conditions such as lymphadenopathy or tuberculosis [14]. In patients with persistent neck swellings that fail to improve with the initial treatments, these cysts must be considered in the differential diagnosis. CT, MRI and histopathology are crucial for its diagnosis. Complete surgical excision is curative and prevents recurrence.
Acknowledgments
We thank the patient for her cooperation and consent to share the clinical details for this report.
Financial Disclosure
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of Interest
The authors declare no conflict of interest related to this case report.
Informed Consent
Informed consent was obtained from the patient for the use of their clinical information and images in this report.
Author Contributions
Dr. Muhammad Uzair: conceptualization, data collection, and primary manuscript drafting. Dr. Husam Jamil: data analysis, manuscript review, and editing.
Data Availability
All relevant data supporting the findings of this case report are included in the manuscript. Additional data can be made available upon request.
Abbreviations
BCA: branchial cleft anomalies; BCC: branchial cleft cyst; SCM: sternocleidomastoid muscle
| References | ▴Top |
- Alshihmani SHA. A second branchial cleft cyst, a case report. Int J Surg Case Rep. 2023;108:108429.
doi pubmed - Acierno SP, Waldhausen JH. Congenital cervical cysts, sinuses and fistulae. Otolaryngol Clin North Am. 2007;40(1):161-176.
doi pubmed - Shen LF, Zhou SH, Chen QQ, Yu Q. Second branchial cleft anomalies in children: a literature review. Pediatr Surg Int. 2018;34(12):1251-1256.
doi pubmed - Paul I, Mohiyuddin SMA, A S, Mohammadi K, Babu P. The outcome of treatment in second branchial cleft anomalies: a case series. Cureus. 2023;15(6):e40164.
doi pubmed - Daoud FS. Branchial cyst: an often forgotten diagnosis. Asian J Surg. 2005;28(3):174-178.
pubmed - Adams A, Mankad K, Offiah C, Childs L. Branchial cleft anomalies: a pictorial review of embryological development and spectrum of imaging findings. Insights Imaging. 2016;7(1):69-76.
doi pubmed - Muller S, Aiken A, Magliocca K, Chen AY. Second branchial cleft cyst. Head Neck Pathol. 2015;9(3):379-383.
doi pubmed - Lee DH, Yoon TM, Lee JK, Lim SC. Clinical study of second branchial cleft anomalies. J Craniofac Surg. 2018;29(6):e557-e560.
doi pubmed - Swarna LR, Nandhini G, Jayant VS, Rajkumar K. Branchial cleft cyst: a case report and literature review. SRM Journal of Research in Dental Sciences. 2017;8(2):88-91.
doi - Khan MA, Bilal W, Asim H, Rahmat ZS, Essar MY, Ahmad S. MDR-TB in Pakistan: Challenges, efforts, and recommendations. Ann Med Surg (Lond). 2022;79:104009.
doi pubmed - Prosser JD, Myer CM, 3rd. Branchial cleft anomalies and thymic cysts. Otolaryngol Clin North Am. 2015;48(1):1-14.
doi pubmed - Chen W, Zhou Y, Xu M, Xu R, Wang Q, Xu H, Chen J, et al. Congenital second branchial cleft anomalies in children: a report of 52 surgical cases, with emphasis on characteristic CT findings. Front Pediatr. 2023;11:1088234.
doi pubmed - Papadogeorgakis N, Petsinis V, Parara E, Papaspyrou K, Goutzanis L, Alexandridis C. Branchial cleft cysts in adults. Diagnostic procedures and treatment in a series of 18 cases. Oral Maxillofac Surg. 2009;13(2):79-85.
doi pubmed - Erkan Gokce, Murat Beyhan. CT and MRI findings of branchial cleft cysts. Eastern Journal of Medicine. 2021;26(1):47-52.
doi
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Current Surgery is published by Elmer Press Inc.