| Journal of Current Surgery, ISSN 1927-1298 print, 1927-1301 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Curr Surg and Elmer Press Inc |
| Journal website https://jcs.elmerpub.com |
Original Article
Volume 000, Number 000, May 2025, pages 000-000
Comparing Pain and Disability Outcomes for Patients Receiving Either Intracostal or Pericostal Closure Technique Following Thoracotomy Incision: Results of a Randomized Trial
Yuvaraj Kotteeswarana, b, f, Alexander McLaren-Bladesb, Maxwell Slepianb, Alexander Huangb, c, Anna Waismand, Joel Katzd, Kazuhiro Yasufukue, Hance Clarkeb, c, f
aDepartment of Anesthesiology, Northern Ontario School of Medicine, Thunder Bay, ON P7B7A5, Canada
bDepartment of Anesthesia and Pain Management, Toronto General Hospital, Toronto, ON M5G 2C4, Canada
cDepartment of Anesthesiology and Pain Medicine, University of Toronto, Toronto, ON M5S 1A1, Canada
dDepartment of Psychology, York University, Toronto, ON M3J 1P3, Canada
eDepartment of Surgery, Division of Thoracic Surgery, Toronto General Hospital, Toronto, ON M5G 2C4, Canada
fCorresponding Author: Yuvaraj Kotteeswaran, Department of Anesthesia and Pain Management, Thunder Bay Regional Health Sciences Centre, Thunder Bay, ON P7B 7A5, Canada; Hance Clarke, Department of Anesthesia and Pain Management, Toronto General Hospital, Toronto, ON M5G 2C4, Canada
Manuscript submitted November 8, 2024, accepted April 4, 2025, published online May 8, 2025
Short title: Thoracotomy Closure Techniques
doi: https://doi.org/10.14740/jcs492
| Abstract | ▴Top |
Background: The association between thoracotomy and intense acute post-surgical pain, as well as the development of post-thoracotomy pain syndrome (PTPS), is well-described. This single-center, double-blinded, randomized controlled trial compared pain and disability after intracostal suture closure versus pericostal suture closure techniques for elective thoracotomy (NCT01898468). Patients were randomized to either intracostal or pericostal closure groups. The primary endpoint was post-surgical acute and chronic pain metrics. Secondary endpoints were patient postoperative opioid consumption, pain-related measures, and quality of life between the groups.
Methods: Adult surgical patients receiving a posterolateral thoracotomy incision were recruited for this study. Exclusion criteria included diagnosis or treatment for: substance use disorder, chronic pain syndromes, acute exacerbation of psychiatric illness, renal impairment, and mesothelioma. Also excluded were patients with a life expectancy of less than 1 year, planned chest wall resection, and elevated rib fracture risk. Standardized anesthesia and analgesic regimens were implemented. Unless contraindicated, all patients received thoracic epidural analgesia. Pain, psychosocial, psychophysical, and quality of life measures were assessed on admission, on hospital discharge, and at 3 months post-surgery.
Results: Thirty-six participants (15 female, mean age = 55.5 (standard deviation (SD) = 16.6)) were recruited and randomized into intracostal and pericostal suture thoracotomy closure groups. Twenty-nine participants completed questionnaires at discharge, and 22 participants completed questionnaires 3 months after surgery. Due to the non-normal distribution of dependent variables (pain intensity, pain-related disability, and morphine milligram equivalent (MME)), non-parametric analyses were performed. There were no differences between groups in opioid consumption during the first 3 days after surgery. Likewise, participants from both closure groups did not differ in pain intensity or pain-related disability at discharge or 3 months after surgery. Pain catastrophizing scores did not differ between groups at any time-point (F(2, 20) = 1.45, P = 0.25).
Conclusion: This study found no difference between the intracostal or pericostal closure groups when measuring pain intensity, pain-related disability, or pain catastrophizing at discharge and 3 months post-discharge. Closure technique did not affect opioid consumption in the first 3 postoperative days.
Keywords: Neuropathic pain; Elective thoracotomy; Intracostal closure; Pericostal closure; Acute post-thoracotomy pain; Postoperative opioid consumption; Pain-related disability; Chronic post-surgical pain
| Introduction | ▴Top |
A thoracotomy incision carries a significant risk of intense acute post-thoracotomy pain and the development of chronic post-surgical pain (CPSP) [1-7]. It has been estimated that the incidence of chronic pain after thoracotomy may be as high as 30% to 70%, which may be attributable to a combination of the acute pain that precedes it and underlying nerve injury. Strategies to improve the acute post-surgical pain experience and limit the development of chronic postoperative pain syndromes are extremely variable, encompassing a variety of regional techniques and analgesic regimes [8-13].
The technique used for rib approximation has been identified as a potential means of improving postoperative pain [14]. Namely, the intracostal closure technique has been recognized as a possible course to avoid pain associated with intercostal nerve impingement. Intracostal rib approximation is accomplished by drilling holes in the inferior rib involved in the closure. Sutures are passed through these holes and over the top of the superior rib involved in the rib approximation. In contrast, pericostal rib approximation is accomplished by securing interrupted sutures over the top of the superior rib and under the inferior rib of the thoracotomy site [15].
The present study compared pericostal and intracostal rib approximation techniques and pain outcomes after posterolateral thoracotomy. The primary endpoint examined how these closure techniques affected the acute post-surgical pain and CPSP. Secondary endpoints examined the comparison of postoperative analgesic consumption, pain-related measures, and quality-of-life metrics of the two surgical closure techniques.
| Materials and Methods | ▴Top |
This was a single-center, double-blinded, randomized controlled trial that compared pain and disability after either intracostal suture closure or pericostal suture closure technique following posterolateral thoracotomy. After Research Ethics Board approval by the University Health Network (REB # 13-5894-B) and registered in CinicalTrials.gov (NCT01898468), patients aged 18 years and older undergoing posterolateral thoracotomy for lung resection at the Toronto General Hospital (a single quaternary care center) between February 2014 and August 2018 were the target population of this study. This study was conducted in compliance with the ethical standards of the responsible institution on human subjects, as well as with the Helsinki Declaration.
All patients provided informed written consent in order to participate in the current study. Patients with a diagnosed drug misuse disorder and those receiving chronic opioid therapy, as well as those with chronic pain syndrome, and psychiatric illness (except depression), were excluded. Patients with chronic renal impairment (a serum creatinine > 104 µmol/L), a life expectancy of less than 12 months, assessed as needing chest wall resection (e.g., those with a diagnosis of mesothelioma), and those deemed to have a higher-than-normal risk of rib fractures (e.g., osteoporosis) were also excluded.
Potential candidates were identified during their clinical appointments with the thoracic surgery and anesthesia pre-surgical assessment clinics at the Toronto General Hospital (Toronto, Ontario). Patients, the research coordinator, and other study personnel were blinded to each patient’s closure group allocation. Members of the surgical team, operating room nurses, and the intraoperative anesthesia team could not be blinded to each patient’s group allocation. However, these persons were not involved in data collection or analysis of the study data.
Closure group allocation (pericostal or intracostal) was randomized. A randomization schedule was created using a web-based randomization program [16] with patients being allotted into the two study arms (pericostal sutures and intracostal sutures).
The surgeon performed the closure technique as described in the randomization log. The patient codes and their group allocations were retained by a statistician not involved in the study. The patient allocations were only revealed after data collection and data entry were completed. Basic demographic and medical history (e.g., comorbidities, operative diagnosis, and planned surgery), as well as baseline pain, psychosocial, depression, and quality of life measures, were recorded. Whenever possible, this information was collected immediately after participant recruitment, with questionnaires being sent home with participants. The initial study questionnaires were collected when patients presented to the hospital for surgery, and the study coordinator was available to assist as needed.
Anesthesia
Participating patients had routine preoperative surgical and anesthesia assessment confirming fitness for surgery. Patients were administered 200 mg of celecoxib by mouth 2 h before surgery. For surgery, large-bore intravenous (IV) access and an arterial line were established. Prior to the induction of anesthesia, a thoracic epidural catheter was placed to facilitate postoperative analgesia. If an epidural could not be placed, it was replaced by IV patient-controlled analgesia (IV PCA) and an extra-pleural catheter for local anesthesia (placed during surgical closure). Barring any contraindications, all patients were administered 1,300 mg of acetaminophen per rectum.
Standard American Society of Anesthesiologists (ASA) monitoring was used during the operations, including both invasive and non-invasive blood pressure monitoring. Induction was accomplished with fentanyl 2 µg/kg, propofol 3 - 5 mg/kg, and rocuronium 1 mg/kg. Sevoflurane was used to maintain anesthesia with a target minimum alveolar concentration (MAC) of 0.8 - 1.2. Intraoperative analgesia consisted of fentanyl titrated to a target of 10 µg/kg, with additional hydromorphone being administered at the discretion of the patient’s anesthesiologist. Intraoperative fluid targets, as well as the decision to administer additional muscle relaxant, were left to the discretion of the patient’s anesthesiologist. Dexamethasone 8 mg IV and granisetron 1 mg IV were used for the prevention of postoperative nausea and vomiting. Patients were not considered for extubation until their measured temperature was at least 36.5 °C.
Thoracotomy technique
All the surgeons involved in this study were capable of performing both intracostal suture closure and pericostal suture closure techniques. Skin incision occurred approximately at the level of the patient’s sixth rib. Incision length was equivalent to the patient’s latissimus dorsi muscle at that level. The muscle was cut, and the underlying serratus anterior muscle was spared with chest entry over the top of the unresected, unshingled, and otherwise intact sixth rib. Electrocautery was used to undercut the top of the sixth rib from the erector spinae fascia to the internal mammary artery. Nerves were injected with bupivacaine via a needle placed into the intercostal muscle surrounding them. After this, the chest retractor was placed and opened slowly to the minimum width required to facilitate surgery. Any rib fractures that occurred were documented and collected by the study personnel. Rib closure (the intervention for this study) was accomplished via classic pericostal suture or intracostal suture. Completion of the appropriate surgical procedure also included placement of one or two 28 French soft chest tubes.
Surgical closure: pericostal sutures
Rib closure was achieved by placing sutures around the ribs in the standard pericostal fashion, with one end of the stitches placed over the top of the fifth rib and the other end of the stitches under the sixth rib.
Surgical closure: intracostal sutures
Evenly placed holes were drilled into the bed of the sixth rib using a 5 mm bit attached to a Stryker drill. Sutures were placed through these holes and looped over the top of the fifth rib before being tied and approximating the rib space.
Postoperative pain management
Postoperative analgesia was administered using epidural patient-controlled epidural analgesia (PCEA) via the patient’s thoracic epidural catheter. In patients who did not receive a thoracic epidural, IV PCA hydromorphone with no basal infusion was administered. All PCA was connected to the patient on their arrival in the post-surgical recovery room or prior to leaving the operating room. IV PCA delivered 0.2 - 0.4 mg of hydromorphone on demand up to a maximum of 10 mg in 4 h. All patients also received celecoxib 200 mg by mouth twice a day for their first 3 postoperative days (unless contraindicated). Further analgesic intervention was left to the discretion of the acute pain service and the managing surgical team. Ambulation and rehabilitation were guided by the surgical team and started as early postoperatively as was appropriate, with day 1 postoperative initiation of these activities being the ideal.
Data collection
The patients enrolled in this study submitted their baseline questionnaires prior to surgery. Pain, pain-related measures, and quality of life metrics were repeated via questionnaire again at discharge, or on the seventh postoperative day (whichever was earlier). At routine follow-up, 3 months postoperatively, all the questionnaires were repeated.
Metrics used for data collection in this study included: 1) the numeric rating scale (NRS). The NRS consists of a series of numbers ranging from 0 to 10 with endpoints representing the most extreme pain experiences (0 = “no pain” and 10 = “worst possible pain” for intensity; and 0 = “not unpleasant” to “most unpleasant sensation imaginable” for pain unpleasantness). Patients choose the number that best corresponds to the intensity and unpleasantness of their pain. The NRS has good reliability and validity and is sensitive to change following pharmacological intervention and to identify genes having a role in chronic pain [17]. 2) McGill Pain Questionnaire-Short Form-2 (SF-MPQ-2). The SF-MPQ-2 [18] is a 22-item, expanded and revised version of the SF-MPQ [19] designed to measure the qualities of neuropathic and non-neuropathic pain. Exploratory and confirmatory factor analyses revealed the presence of the following four factors or subscales: continuous pain, intermittent pain, neuropathic pain, and affective pain descriptor. Preliminary analyses indicate that the SF-MPQ-2 has very good to excellent psychometric properties. 3) Pain catastrophizing scale (PCS). Pain catastrophizing is a negative cognitive-affective response to pain (actual or anticipated) that has been linked to pain-related outcomes [20]. The PCS examines three components of catastrophizing (rumination, magnification, and helplessness) using a 13-item questionnaire [21]. 4) Pain disability index (PDI). The PDI is a 7-item questionnaire assessing the magnitude of self-reported disability due to pain in areas such as work, leisure, and sports. This questionnaire has moderate-to-good reliability and good concurrent validity with the Oswestry Disability Questionnaire [22].
Outcomes
Primary outcome
The primary outcome compared the intensity of acute post-surgical pain and CPSP between pericostal and intracostal surgical closure techniques.
Secondary outcomes
Secondary outcome measures sought to compare postoperative opioid consumption during the first 3 days after surgery, differences in psychological measures, and quality of life.
Data analysis
All outcome variables were evaluated for normality prior to analysis. Examination of skewness and kurtosis revealed that participant responses on the MPQ-SF-2, PDI, and PCS were not normally distributed. As such, analyses involving these variables were conducted using non-parametric independent-samples Kruskal-Wallis tests. For normally distributed outcome variables, linear mixed effects models were used to examine the impact of closure types on perioperative and postoperative outcomes. In all mixed effects models, closure type was included as a between-groups factor, and time was entered as a repeated factor (three levels: postoperative days 0 - 2 or baseline, discharge, 3 months) with a first-order autoregressive covariance structure.
| Results | ▴Top |
Sample characteristics
Thirty-six participants (15 female, mean age = 55.5 (standard deviation (SD) = 16.6) were randomized to intracostal suture closure (group 1, n = 17) or pericostal suture closure (group 2, n = 19) (Fig. 1) and completed measures before surgery. Twenty-nine participants (14 female) completed measures at discharge, and 22 participants (13 female) completed measures 3 months after surgery. The majority of participants in both groups were diagnosed with primary lung cancer (80%), followed in frequency by lung metastases (14%), thymoma (3%), and hydatid cyst (3%). Relevant health history included hypertension (34%), hypercholesterolemia (8%), myocardial infarction (6%), congestive heart failure (3%), angina (8%), and smoking history (56%). Health history did not differ between groups (P > 0.05). No differences were found between the groups for the intraoperative drugs used, including analgesics and muscle relaxants. On average, patients ambulated less than 2 days after surgery and stayed in the hospital for 6 days after surgery. There were no differences between closure techniques (Table 1). Ninety-three-point nine percent of patients were seen by the acute pain service for an average of 3.5 days. Across groups, eight participants (26.2%) reported, on average, moderate or severe pain (NRS ≥ 4) during the first 2 days after surgery, and the average daily consumption of opioids was 13.4 MME (Table 1).
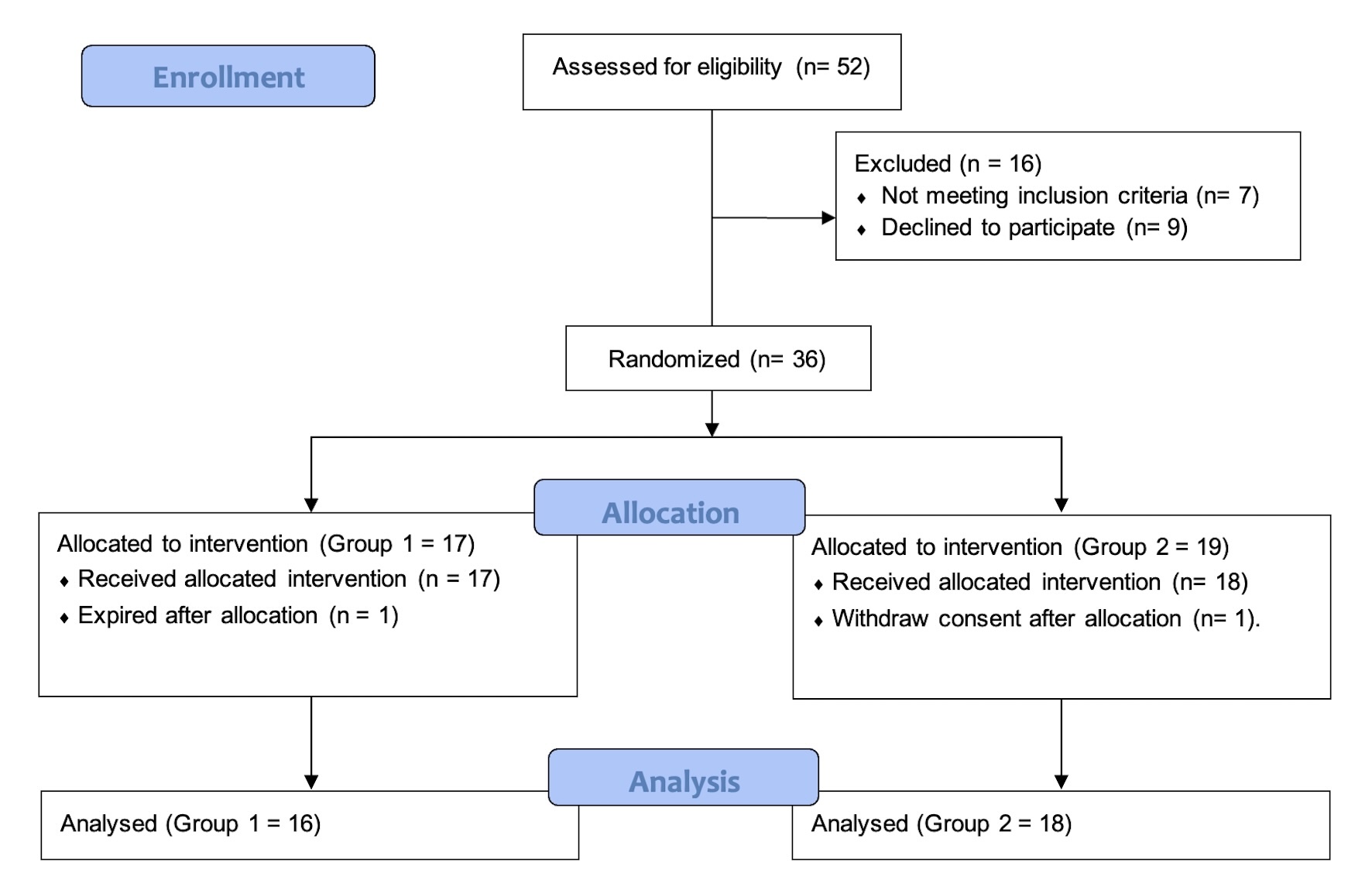 Click for large image | Figure 1. CONSORT flow diagram of the study population. |
 Click to view | Table 1. In-Hospital Descriptive Statistics |
Pain intensity ratings (SF-MPQ-2), pain-related disability (PDI), and pain catastrophizing (PCS) at baseline, discharge, and 3-month follow-up are demonstrated in Table 2. Six patients (20.7%) reported moderate to severe pain intensity at discharge, whereas zero patients reported moderate or severe pain after 3 months. The majority of patients (65.5%) reported at least moderate pain-related disability at discharge (PDI ≥ 27), and three (9%) patients maintained these ratings 3 months later. Four participants (12%) scored above a risk cutoff on the PCS (total score > 24) at baseline, and two of these patients (6%) continued to score above this cutoff at discharge and 3 months later.
 Click to view | Table 2. Pain Intensity, Pain Disability, and Pain Catastrophizing at Baseline, Discharge, and 3 Months Post-Surgery |
Impact of surgical closure on pain outcomes
Linear mixed effects models were used to examine the impact of closure type on pain at rest and during movement over the first 3 postoperative days. Pain at rest did not differ between closure type groups over the first 3 days after surgery (F(2, 59.54) = 1.61, P = 0.21). Similarly, there were no differences in pain during movement between closure type groups over the first 3 days after surgery (F(2, 58.22) = 2.23, P = 0.12). Pain intensity did not differ between groups at baseline (Χ2(1) = 0.23, P = 0.81), discharge (Χ2(1) = 0.01, P = 0.86), or 3 months after surgery (Χ2(1) = 1.22, P = 0.27).
Impact of surgical closure on analgesic use, pain-related disability, and pain catastrophizing
Linear mixed effects models were used to examine the impact of closure type on opioid consumption over the first 3 postoperative days. Opioid consumption did not differ between closure type groups over the first 3 days after surgery (F(2,70.63) = 0.57, P = 0.57).
Pain-related disability did not differ between groups at baseline (Χ2(1) = 0.48, P = 0.49), discharge (Χ2(1) = 0.33, P = 0.57), or 3 months after surgery (Χ2(1) = 1.56, P = 0.21). Pain catastrophizing did not differ between groups at baseline (Χ2(1) = 2.64, P = 0.10), discharge (Χ2(1) = 0.04, P = 0.84), or 3 months after surgery (Χ2(1) = 0.06, P = 0.81).
| Discussion | ▴Top |
Pain after thoracotomy has been described as intense and is known to be associated with a high incidence of post-thoracotomy pain syndrome (PTPS). PTPS in particular is estimated to have an incidence of 15% to 67% [1-3]. Post-thoracotomy pain is likely the result of a complex process involving intraoperative and postoperative nociception, central sensitization, and nerve injury [9, 23]. The intercostal nerve has been observed as being potentially vulnerable to injury during the rib retraction and rib approximation necessary for thoracotomy. Because of this, strategies and techniques have evolved to limit intercostal nerve injury and potentially reduce its contribution to the acute and chronic postoperative pain experience of thoracotomy patients [23].
Due to the above-mentioned incidence of thoracotomy incisions causing CPSP, our thoracic surgery division changed its practice to circumvent the thoracotomy incision and moved almost exclusively to video-assisted thoracoscopic procedures. This resulted in difficulty recruiting patients to our study. As pointed out in an editorial by Katz [24], unanticipated changes to the way thoracic surgery was practiced during the course of the trial appear to have contributed to greater difficulty recruiting the required number of participants, as mentioned in clinicaltrial.org (NCT01898468). It is surprising to note that between 30% and 50% of clinical trials never get published [25, 26]. Consistent with this literature, Katz reported that the most common reasons for trial discontinuation and non-publication are difficulty recruiting the required sample size [27]. Non-publication can result in publication bias characterized by the presence of non-random differences between the published and non-published literature.
For example, studies reporting statistically significant results are twice as likely to get published as those with nonsignificant findings, and effect sizes of published studies are greater than unpublished studies. The consequences of this publication bias include inaccurate results of systematic reviews, wasted resources, a threat to the evidence-based literature, and potential harm to patients [28, 29].
As is evident in Table 2, no significant differences were found between the surgical closure techniques in terms of pain intensity, pain-related disability, or pain catastrophizing. This may suggest that the rib approximation technique alone does not play a major role in the development of CPSP. However, we concede that this finding may be due to a lack of adequate sample size, given the change in practice at our institution at the outset of this work. Consequently, the ideal way to achieve complete pain relief for patients after thoracotomy remains unknown. At present, the best approach would be to start pain relief for patients preoperatively and continue throughout the perioperative and postoperative stages, including after discharge, through the care that is provided via the implementation of transitional pain services [30-33].
There have been several studies examining the effect of rib approximation technique on post-thoracotomy pain outcomes [12, 34, 35]. However, many of these studies have been small, and very few have been blinded or randomized.
One of the largest studies examining pain outcomes and thoracotomy closure technique was conducted by Cerfolio et al (2003). This study recruited 280 consecutive patients undergoing thoracotomy. The first 140 patients had pericostal rib approximation, while the remaining 140 patients had intracostal rib approximation. All patients received pre-induction epidural placement. Patients with non-functioning epidurals or no epidurals were excluded from the study, as were patients with chronic pain conditions. Pain scores in the pericostal group were significantly higher 2 weeks, 1 month, 2 months, and 3 months after surgery. The pericostal group was also more likely to describe their pain as hot/burning, shooting, or stabbing [34].
Leandro et al (2014) compared pericostal and transcostal (intracostal) rib approximation for thoracotomy closure in a prospective, randomized, double-blind study consisting of 30 patients (pericostal n = 16, transcostal n = 14). Their primary outcomes were postoperative pain and lung function. They noted significantly greater perioperative pain, as recorded by visual analogue scale (VAS) and McGill Pain Questionnaire metrics, in the pericostal group [35].
Bayram et al (2011) randomized patients into an intracostal group or a group with holes drilled into the superior and inferior rib involved in rib approximation. In the latter, group sutures were passed through the hole in the superior and inferior rib and used to approximate the ribs. Thirty patients were enrolled in each arm of the study, and all patients had pre-induction epidural placement and postoperative PCEA. This study reported that patients in the non-intracostal group had significantly lower PCEA analgesia consumption, VAS scores at rest and with coughing, and observer verbal ranking scale (OVRS) compared to the other group. The investigators concluded that thoracotomy closure that further avoided intercostal nerve injury (by approximating ribs through superior and inferior holes drilled in them) significantly decreased post-thoracotomy pain [12].
The studies described above are similar to the one presented in this paper. These studies suggest that avoidance of intercostal nerve compression should reduce postoperative pain and that greater effort to avoid intercostal nerve compression may have additional benefit. However, these findings were not reproduced in our study, with both the intracostal and pericostal groups showing similar pain-related outcomes. Of importance, it should be noted that none of these studies took pain-related measures or quality of life metrics into consideration.
Limitations
Our study was limited by its small sample size, as well as due to difficulty recruiting a sample size due to the above-mentioned reasons. There also may have been uncontrolled but significant differences between the intracostal and pericostal study populations. A much larger sample size would be required to determine the significance of the two thoracotomy closure techniques on pain outcomes.
Conclusions
In conclusion, we present the results of a double-blinded randomized controlled trial comparing pain and pain-related disability outcomes after either pericostal or intracostal rib approximation techniques for posterolateral thoracotomy. The pericostal and intracostal closure groups were comparable. There was no significant difference between the demographic data and pain catastrophization of these groups in the preoperative period. A uniform anesthetic and surgical technique was delivered to both groups. Ultimately, no significant difference was found between the rib approximation groups regarding opioid consumption, pain intensity, or pain-related disability measures. Our results suggest that during thoracotomy, intercostal nerve injury and nociception that occur prior to rib approximation may be of greater significance to pain and pain-related disability outcomes than the rib approximation technique alone. However, given the complexity of post-thoracotomy pain and varying findings from other studies, strategies aimed at protecting the intercostal nerve and removing its contribution deserve future investigation.
Acknowledgments
None to declare.
Financial Disclosure
This study was supported by a grant provided by Physician Services Incorporated.
Conflict of Interest
None to declare.
Informed Consent
All patients provided informed written consent to participate in the current study.
Author Contributions
Yuvaraj Kotteeswaran helped to arrange the data, review the literature, and write the manuscript. Alexander McLaren-Blades helped to review the literature and write the manuscript. Maxwell Slepian helped to analyze the data and write the manuscript. Alexander Huang helped to write the manuscript. Anna Waisman helped to write and edit the manuscript. Joel Katz helped to edit the manuscript and oversee the study. Kazuhiro Yasufuku helped to perform surgery and write the manuscript. Hance Clarke helped to design the study, perform the randomization, analyze the data, review the literature, and write the manuscript.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
ASA: American Society of Anesthesiologists; CPSP: chronic post-surgical pain; MAC: minimum alveolar concentration; MME: morphine milligram equivalent; NRS: numeric rating scale; OVRS: observer verbal ranking scale; PCA: patient-controlled analgesia; PCEA: patient-controlled epidural analgesia; PCS: pain catastrophizing scale; PDI: pain disability index; PTPS: post-thoracotomy pain syndrome; REB: Research Ethics Board; SF-MPQ-2: McGill Pain Questionnaire-Short Form-2; UHN: University Health Network; VAS: visual analogue scale
| References | ▴Top |
- Kalso E, Perttunen K, Kaasinen S. Pain after thoracic surgery. Acta Anaesthesiol Scand. 1992;36(1):96-100.
doi pubmed - Guastella V, Mick G, Soriano C, Vallet L, Escande G, Dubray C, Eschalier A. A prospective study of neuropathic pain induced by thoracotomy: incidence, clinical description, and diagnosis. Pain. 2011;152(1):74-81.
doi pubmed - Perttunen K, Tasmuth T, Kalso E. Chronic pain after thoracic surgery: a follow-up study. Acta Anaesthesiol Scand. 1999;43(5):563-567.
doi pubmed - Katz J, Jackson M, Kavanagh BP, Sandler AN. Acute pain after thoracic surgery predicts long-term post-thoracotomy pain. Clin J Pain. 1996;12(1):50-55.
doi pubmed - Katz J, Asmundson GJ, McRae K, Halket E. Emotional numbing and pain intensity predict the development of pain disability up to one year after lateral thoracotomy. Eur J Pain. 2009;13(8):870-878.
doi pubmed - Marshall K, McLaughlin K. Pain management in thoracic surgery. Thorac Surg Clin. 2020;30(3):339-346.
doi pubmed - Liu CW, Page MG, Weinrib A, Wong D, Huang A, McRae K, Fiorellino J, et al. Predictors of one year chronic post-surgical pain trajectories following thoracic surgery. J Anesth. 2021;35(4):505-514.
doi pubmed - Humble SR, Dalton AJ, Li L. A systematic review of therapeutic interventions to reduce acute and chronic post-surgical pain after amputation, thoracotomy or mastectomy. Eur J Pain. 2015;19(4):451-465.
doi pubmed - Rodriguez-Aldrete D, Candiotti KA, Janakiraman R, Rodriguez-Blanco YF. Trends and new evidence in the management of acute and chronic post-thoracotomy pain-an overview of the literature from 2005 to 2015. J Cardiothorac Vasc Anesth. 2016;30(3):762-772.
doi pubmed - Kelsheimer B, Williams C, Kelsheimer C. New emerging modalities to treat post-thoracotomy pain syndrome: a review. Mo Med. 2019;116(1):41-44.
pubmed - Katz J, Seltzer Z. Transition from acute to chronic postsurgical pain: risk factors and protective factors. Expert Rev Neurother. 2009;9(5):723-744.
doi pubmed - Bayram AS, Ozcan M, Kaya FN, Gebitekin C. Rib approximation without intercostal nerve compression reduces post-thoracotomy pain: a prospective randomized study. Eur J Cardiothorac Surg. 2011;39(4):570-574.
doi pubmed - Wang L, Yang M, Meng W. Prevalence and characteristics of persistent postoperative pain after thoracic surgery: a systematic review and meta-analysis. Anesth Analg. 2023;137(1):48-57.
doi pubmed - Visagan R, McCormack DJ, Shipolini AR, Jarral OA. Are intracostal sutures better than pericostal sutures for closing a thoracotomy? Interact Cardiovasc Thorac Surg. 2012;14(6):807-815.
doi pubmed - Ranganathan P, Jiwnani S, Pramesh CS. Intercostal nerve protection to prevent post-thoracotomy pain. J Thorac Dis. 2019;11(Suppl 9):S1434-S1435.
doi pubmed - Randomization.com. Available from: http://www.jerrydallal.com/random/randomize.htm.
- Katz J, Melzack R. Measurement of pain. Surg Clin North Am. 1999;79(2):231-252.
doi pubmed - Dworkin RH, Turk DC, Revicki DA, Harding G, Coyne KS, Peirce-Sandner S, Bhagwat D, et al. Development and initial validation of an expanded and revised version of the Short-form McGill Pain Questionnaire (SF-MPQ-2). Pain. 2009;144(1-2):35-42.
doi pubmed - Melzack R. The short-form McGill Pain Questionnaire. Pain. 1987;30(2):191-197.
doi pubmed - Quartana PJ, Campbell CM, Edwards RR. Pain catastrophizing: a critical review. Expert Rev Neurother. 2009;9(5):745-758.
doi pubmed - Osman A, Barrios FX, Kopper BA, Hauptmann W, Jones J, O'Neill E. Factor structure, reliability, and validity of the Pain Catastrophizing Scale. J Behav Med. 1997;20(6):589-605.
doi pubmed - Gronblad M, Hupli M, Wennerstrand P, Jarvinen E, Lukinmaa A, Kouri JP, Karaharju EO. Intercorrelation and test-retest reliability of the Pain Disability Index (PDI) and the Oswestry Disability Questionnaire (ODQ) and their correlation with pain intensity in low back pain patients. Clin J Pain. 1993;9(3):189-195.
doi pubmed - Buchheit T, Pyati S. Prevention of chronic pain after surgical nerve injury: amputation and thoracotomy. Surg Clin North Am. 2012;92(2):393-407.
doi pubmed - Katz J. Editor's corner: negative trials and tribulations. Can J Pain. 2019;3(1):178-179.
doi pubmed - Pica N, Bourgeois F. Discontinuation and nonpublication of randomized clinical trials conducted in children. Pediatrics. 2016;138(3):e20160223.
doi pubmed - Song F, Parekh S, Hooper L, Loke YK, Ryder J, Sutton AJ, Hing C, et al. Dissemination and publication of research findings: an updated review of related biases. Health Technol Assess. 2010;14(8):.
doi pubmed - Huang GD, Bull J, Johnston McKee K, Mahon E, Harper B, Roberts JN, CTTI Recruitment Project Team. Clinical trials recruitment planning: A proposed framework from the Clinical Trials Transformation Initiative. Contemp Clin Trials. 2018;66:74-79.
doi pubmed - Murad MH, Chu H, Lin L, Wang Z. The effect of publication bias magnitude and direction on the certainty in evidence. BMJ Evid Based Med. 2018;23(3):84-86.
doi pubmed - Every-Palmer S, Howick J. How evidence-based medicine is failing due to biased trials and selective publication. J Eval Clin Pract. 2014;20(6):908-914.
doi pubmed - Katz J, Weinrib A, Fashler SR, Katznelzon R, Shah BR, Ladak SS, Jiang J, et al. The Toronto general hospital transitional pain service: development and implementation of a multidisciplinary program to prevent chronic postsurgical pain. J Pain Res. 2015;8:695-702.
doi pubmed - Weinrib AZ, Azam MA, Birnie KA, Burns LC, Clarke H, Katz J. The psychology of chronic post-surgical pain: new frontiers in risk factor identification, prevention and management. Br J Pain. 2017;11(4):169-177.
doi pubmed - Mikhaeil J, Ayoo K, Clarke H, Wasowicz M, Huang A. Review of the Transitional Pain Service as a method of postoperative opioid weaning and a service aimed at minimizing the risk of chronic post-surgical pain. Anaesthesiol Intensive Ther. 2020;52(2):148-153.
doi pubmed - Abrams BA, Murray KA, Mahoney K, Raymond KM, McWilliams SK, Nichols S, Mahmoudi E, et al. Postdischarge pain management after thoracic surgery: a patient-centered approach. Ann Thorac Surg. 2020;110(5):1714-1721.
doi pubmed - Cerfolio RJ, Price TN, Bryant AS, Sale Bass C, Bartolucci AA. Intracostal sutures decrease the pain of thoracotomy. Ann Thorac Surg. 2003;76(2):407-411; discussion 411-402.
doi pubmed - Leandro JD, Rodrigues OR, Slaets AF, Schmidt AF, Jr., Yaekashi ML. Comparison between two thoracotomy closure techniques: postoperative pain and pulmonary function. J Bras Pneumol. 2014;40(4):389-396.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Current Surgery is published by Elmer Press Inc.