Comparing Pain and Disability Outcomes for Patients Receiving Either Intracostal or Pericostal Closure Technique Following Thoracotomy Incision: Results of a Randomized Trial
DOI:
https://doi.org/10.14740/jcs492Keywords:
Neuropathic pain, Elective thoracotomy, Intracostal closure, Pericostal closure, Acute post-thoracotomy pain, Postoperative opioid consumption, Pain-related disability, Chronic post-surgical painAbstract
Background: The association between thoracotomy and intense acute post-surgical pain, as well as the development of post-thoracotomy pain syndrome (PTPS), is well-described. This single-center, double-blinded, randomized controlled trial compared pain and disability after intracostal suture closure versus pericostal suture closure techniques for elective thoracotomy (NCT01898468). Patients were randomized to either intracostal or pericostal closure groups. The primary endpoint was post-surgical acute and chronic pain metrics. Secondary endpoints were patient postoperative opioid consumption, pain-related measures, and quality of life between the groups.
Methods: Adult surgical patients receiving a posterolateral thoracotomy incision were recruited for this study. Exclusion criteria included diagnosis or treatment for: substance use disorder, chronic pain syndromes, acute exacerbation of psychiatric illness, renal impairment, and mesothelioma. Also excluded were patients with a life expectancy of less than 1 year, planned chest wall resection, and elevated rib fracture risk. Standardized anesthesia and analgesic regimens were implemented. Unless contraindicated, all patients received thoracic epidural analgesia. Pain, psychosocial, psychophysical, and quality of life measures were assessed on admission, on hospital discharge, and at 3 months post-surgery.
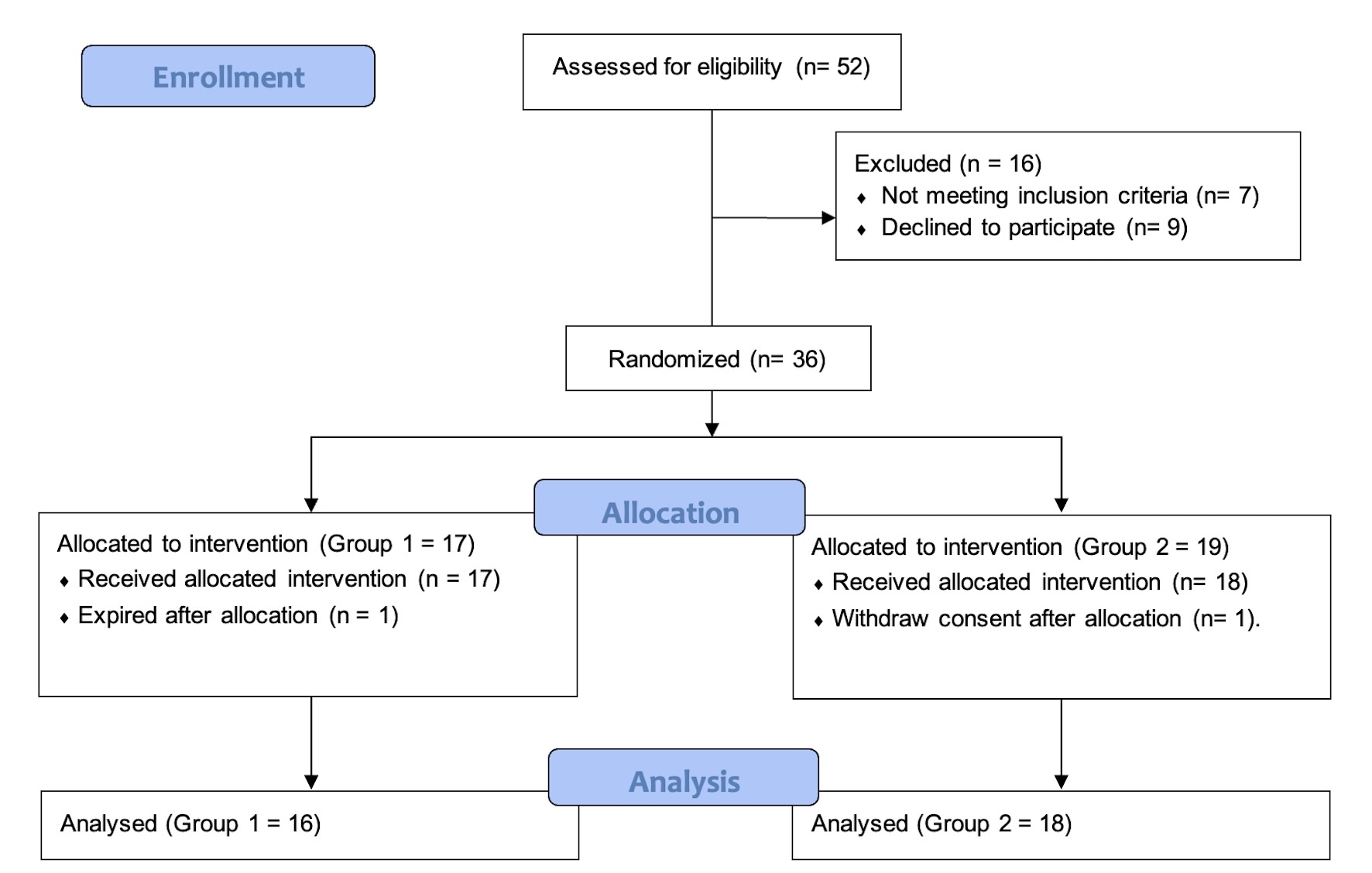
Results: Thirty-six participants (15 female, mean age = 55.5 (standard deviation (SD) = 16.6)) were recruited and randomized into intracostal and pericostal suture thoracotomy closure groups. Twenty-nine participants completed questionnaires at discharge, and 22 participants completed questionnaires 3 months after surgery. Due to the non-normal distribution of dependent variables (pain intensity, pain-related disability, and morphine milligram equivalent (MME)), non-parametric analyses were performed. There were no differences between groups in opioid consumption during the first 3 days after surgery. Likewise, participants from both closure groups did not differ in pain intensity or pain-related disability at discharge or 3 months after surgery. Pain catastrophizing scores did not differ between groups at any time-point (F(2, 20) = 1.45, P = 0.25).
Conclusion: This study found no difference between the intracostal or pericostal closure groups when measuring pain intensity, pain-related disability, or pain catastrophizing at discharge and 3 months post-discharge. Closure technique did not affect opioid consumption in the first 3 postoperative days.
Published
Issue
Section
License
Copyright (c) 2025 The authors

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.





