| Journal of Current Surgery, ISSN 1927-1298 print, 1927-1301 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Curr Surg and Elmer Press Inc |
| Journal website https://www.currentsurgery.org |
Review
Volume 000, Number 000, December 2024, pages 000-000
Clinical Presentation, Diagnostic Approach, and Management of Symptomatic Gastrointestinal Lipomas
Lefika Bathobakaea, h , Heba Farhanb, Tyler Wilkinsonc, Dina Rohirad, Trevor Ruffd, Nischal Sharmae, Kamal Amerf, Yana Cavanaghf, g, Walid Baddouraf
aDepartment of Internal Medicine, St. Joseph’s University Medical Center, Paterson, NJ, USA
bRowan-Virtua University School of Osteopathic Medicine, Stratford, NJ, USA
cDepartment of Family Medicine, Union Hospital, Terre Haute, IN, USA
dSt. George’s University School of Medicine, Grenada, West Indies
eDepartment of Internal Medicine, SUNY Downstate Health Sciences University, Brooklyn, NY, USA
fDepartment of Gastroenterology & Hepatology, St. Joseph’s University Medical Center, Paterson, NJ, USA
gDepartment of Interventional & Surgical Endoscopy, St. Joseph’s University Medical Center, Paterson, NJ, USA
hCorresponding Author: Lefika Bathobakae, Department of Internal Medicine, St. Joseph’s University Medical Center, Paterson, NJ, USA
Manuscript submitted July 15, 2024, accepted July 22, 2024, published online September 16, 2024
Short title: Symptomatic Gastrointestinal Lipomas
doi: https://doi.org/10.14740/jcs482
- Abstract
- Introduction
- Epidemiology
- Etiopathogenesis
- Clinical Manifestations
- Diagnosis
- Treatment and Outcomes
- Conclusion
- References
| Abstract | ▴Top |
Gastrointestinal (GI) lipomas are a rare form of benign submucosal neoplasm composed of mature adipose tissue. These lesions can grow anywhere in the GI tract, with a higher prevalence observed in the colon and the small intestines. Owing to their relative rarity and asymptomatic nature, the true incidence and prevalence remain unknown. GI lipomas can present with dysphagia, abdominal pain, intestinal obstruction, or GI bleeding, prompting further workup and interventions. On computed tomography and magnetic resonance imaging, GI lipomas typically appear as ovoid/spherical, sharply demarcated, and homogeneously hypodense lesions. On endoscopy, lipomas appear as smooth mucosal protrusions and, rarely, with ulceration. In some cases, an endoscopic ultrasound may be used to confirm diagnosis, staging, or pre-operative planning. Asymptomatic lipomas are managed conservatively using periodic imaging or endoscopy. Symptomatic lipomas, however, require endoscopic or surgical resection, and endoscopic techniques are preferred because of their non-invasive nature. Surgery is typically reserved for giant lipomas or more complex cases. There is a paucity of data regarding the clinical features and management of symptomatic GI lipomas. The current evidence is retrospective, in the form of case reports and conference abstracts. In this review, we discuss the clinical presentation, diagnostic approach, and management of symptomatic GI lipomas.
Keywords: Gastrointestinal lipomas; Esophageal lipoma; Gastric lipoma; Intestinal lipoma; Colonic lipoma; Subepithelial lesions; Endoscopic resection
| Introduction | ▴Top |
Gastrointestinal (GI) lipomas are rare benign tumors composed mainly of mature adipose tissue, occurring anywhere in the GI tract [1-3]. These subepithelial lesions are relatively uncommon, with an estimated incidence of 0.035% and 4.4% in autopsy series [1, 4], making up 3% of all GI tumors [2]. GI lipomas commonly occur in the colon and small intestine, and rarely in the stomach and esophagus [5-7]. The etiopathogenesis of these lesions remains unclear, though some studies suggest a possible genetic predisposition [8, 9]. Most GI lipomas are asymptomatic and are often discovered incidentally during imaging or endoscopic procedures for unrelated conditions [10]. When symptomatic, they may present with dysphagia, abdominal pain, GI bleeding, altered bowel habits, intestinal obstruction, or intussusception [3, 11-15].
Diagnosing GI lipomas often involves a combination of radiological studies and endoscopy. Endoscopy allows direct visualization and biopsy of the lesions for histopathological analysis. Asymptomatic lipomas usually do not require treatment and can be monitored with regular follow-ups. Symptomatic lipomas, however, may necessitate endoscopic or surgical resection, depending on their location and severity of the symptoms [15]. There is a paucity of data on the clinical manifestations and management of symptomatic GI lipomas. Current evidence is anecdotal, in the form of case reports and conference abstracts. Owing to their rarity, indolent nature, and vague presentation, GI lipomas can simulate malignant lesions, creating a diagnostic and therapeutic dilemma for clinicians [3]. This narrative review describes the clinical presentation, diagnostic approach, and management of symptomatic GI lipomas.
| Epidemiology | ▴Top |
A lipoma is a benign tumor predominantly composed of mature adipose tissue, typically presenting as a soft, pliable, and well-defined mass [2, 4, 7, 16]. These tumors vary in size, ranging from a few millimeters to several centimeters, and are usually yellowish with a smooth surface [6]. GI lipomas are most often located in the submucosa layer and can be found anywhere in the GI tract, although they are most common in the colon and small intestine [6, 7]. They may be sessile or pedunculated [4], influencing their mobility and potential to cause obstructive symptoms. Occasionally, larger lipomas may show signs of necrosis or surface ulceration, especially if subjected to chronic irritation [7].
Esophageal lipomas are rare benign tumors, accounting for less than 1% of all esophageal tumors [17-20]. Their distribution along the esophagus varies, but they are often found in the upper or middle third of the esophagus [16, 17, 20]. The rarity and often asymptomatic presentation of esophageal lipomas make epidemiological studies challenging, and most of the current knowledge comes from case reports and small case series. In a systematic review of esophageal lipomas and liposarcomas from 1955 to 2020, Ferrari et al [17] identified 65 case reports and two review articles comprising 239 patients. Of these, 176 had an esophageal lipoma, with the cervical esophagus being the most common location [17].
Gastric lipomas account for 3-5% of all GI lipomas and less than 1% of all gastric tumors [21, 22]. These tumors can be found anywhere in the stomach, but are most frequently located in the antrum (Fig. 1) [2, 22]. The size of gastric lipomas can vary considerably, ranging from a few millimeters to several centimeters in diameter. Although many gastric lipomas remain asymptomatic, larger tumors can cause a variety of obstructive or dyspeptic symptoms.
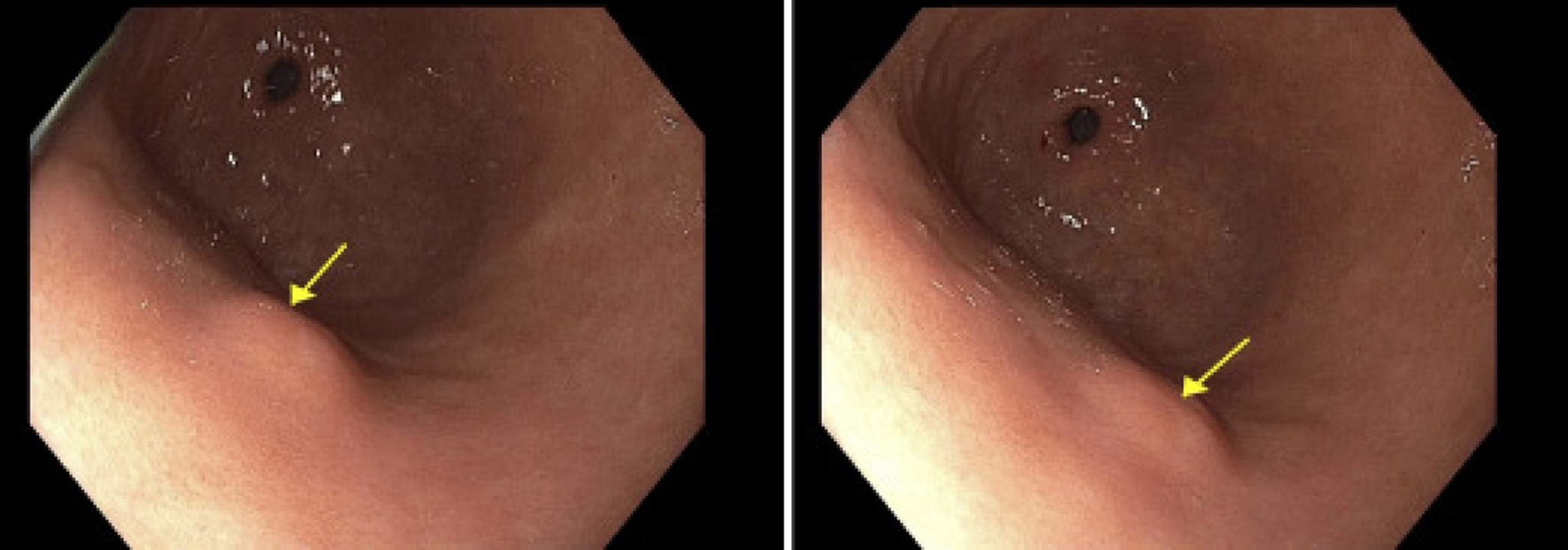 Click for large image | Figure 1. Endoscopic image showing a single 8 mm submucosal nodule (arrows) on the anterior wall of the gastric body. The lesion appeared hyperechoic on endoscopic ultrasound and invaded into the submucosa (layer 3). |
Small intestinal lipomas are among the most common benign tumors of the small intestine; however, they represent only a small fraction of all GI tumors (Fig. 2). These tumors are most prevalent in adults aged 50 - 70 years, with a slight male predominance [23]. Their exact incidence is difficult to determine, as many remain asymptomatic and undetected, discovered only incidentally during imaging, endoscopy, or surgeries. A systematic review of symptomatic small bowel lipomas of the jejunum and ileum from 2000 to 2019 yielded 142 articles, totaling 147 patients [1]. There were 138 adults and nine pediatric patients with a mean age of 49.9 years [1].
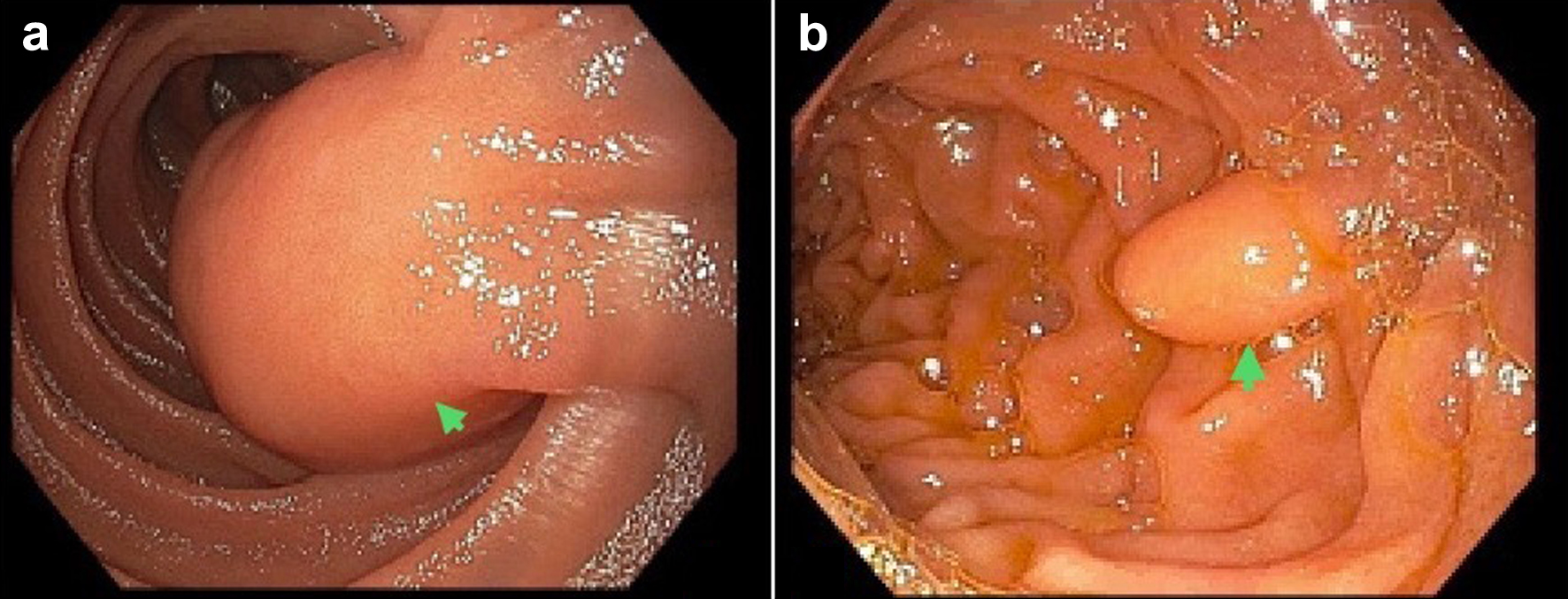 Click for large image | Figure 2. Endoscopic images illustrating lipomas in the small intestines. (a) A mass in the third portion of the duodenum (arrow). Histopathology was consistent with a duodenal lipoma. (b) A medium-sized lipoma, measuring 12 mm in diameter, in the second portion of the duodenum (arrow). |
Colorectal lipomas are more common and typically manifest in the colon, particularly in the submucosal layer, but can also occur in the rectum (Fig. 3) [24, 25]. Although colorectal lipomas are benign and often asymptomatic, their identification is clinically relevant, especially when they become large enough to cause obstruction, bleeding, or intussusception [12, 13, 26]. In a systematic review of large colonic lipomas, Crocetti et al [26] discovered 70 pertinent articles consisting of 126 patients. There was a slight female predominance, and the average patient age was 61.9 years.
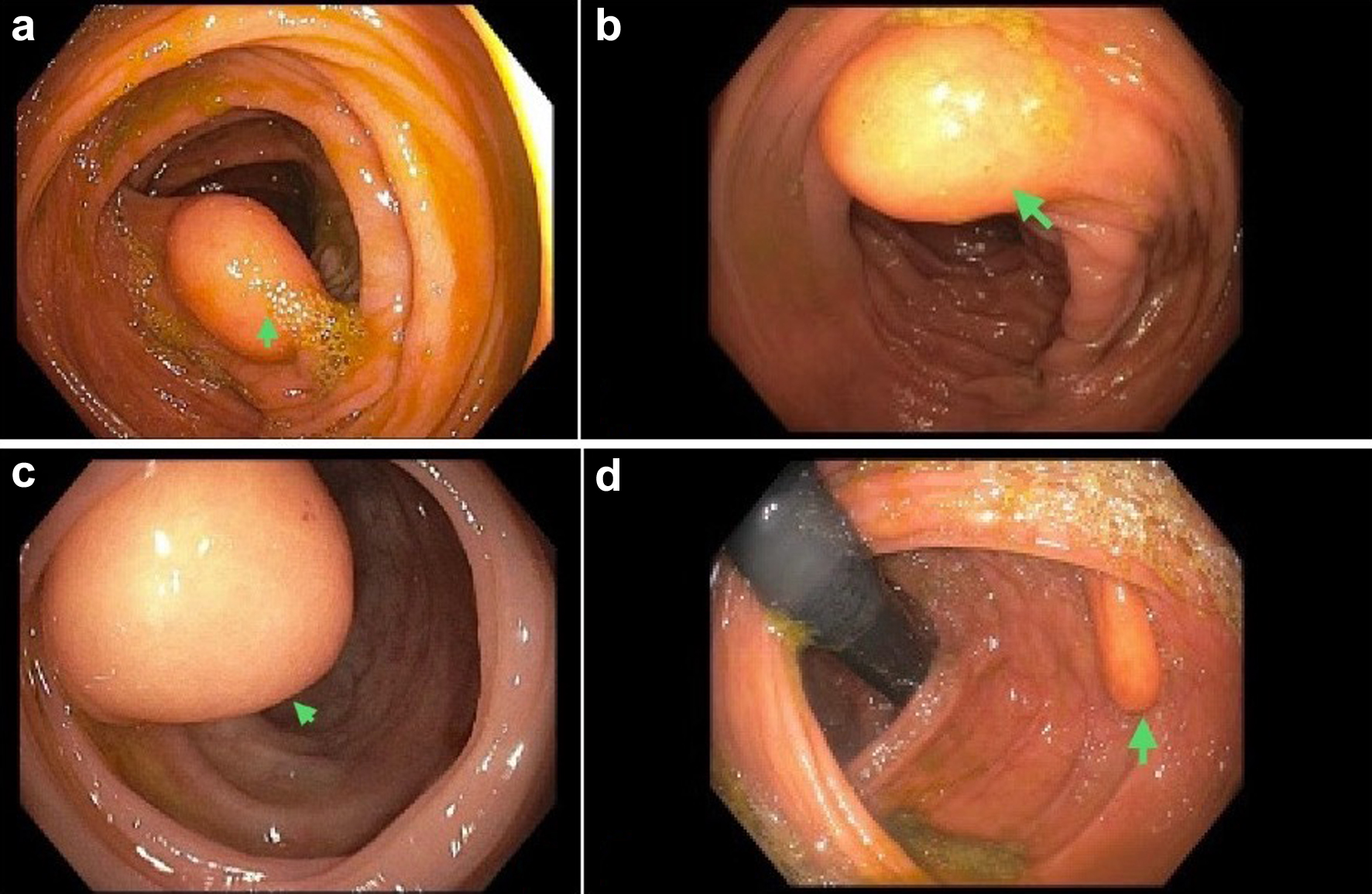 Click for large image | Figure 3. A library of endoscopic images showing colorectal lipomas. (a) A large lipoma, measuring 15 mm in diameter, in the ascending colon. (b) A medium-sized lipoma at the hepatic flexure. (c) A large lipoma at the ileocecal valve. (d) A medium-sized lipoma at the splenic flexure, in the transverse and ascending colon. |
| Etiopathogenesis | ▴Top |
The exact etiology and pathogenesis of GI lipomas remain largely unclear, though several theories have been proposed. One hypothesis suggests that they arise from adipocytes in the submucosa or subserosa due to chronic irritation or inflammation, which stimulates adipose tissue proliferation [9, 16, 26]. Another theory posits a developmental origin, where lipomas develop from sequestered adipose tissue remnants that proliferate abnormally [2, 9, 26]. Genetic factors may also play a role; for instance, mutations in genes regulating adipocyte growth could predispose individuals to lipoma formation [8, 9]. Additionally, some studies have suggested an association with obesity and hyperlipidemia, indicating a possible metabolic influence on the growth of these tumors [27]. The benign nature of GI lipomas means that they generally have limited clinical significance unless they reach a size or location that leads to symptoms. Understanding their epidemiology, etiopathogenesis, and clinical manifestations is crucial to improve diagnostic accuracy and patient outcomes.
| Clinical Manifestations | ▴Top |
Symptomatic GI lipomas can present with a range of clinical manifestations depending on the lesion size and location. Esophageal lipomas can cause dysphagia, odynophagia, chest pain, weight loss, regurgitation, and, in rare cases, aspiration [17, 19, 20]. These symptoms arise primarily from the mechanical obstruction caused by larger tumors, and treatment depends on the severity of the symptoms. Gastric lipomas are usually incidental findings on imaging or endoscopy, but symptomatic cases may present with abdominal pain, hematemesis, melena, gastric outlet obstruction, and dyspepsia [2, 5, 22]. Owing to their vague presentation, gastric lipomas can simulate peptic ulcers, GI stromal tumors (GISTs), or gastric cancer, prompting further diagnostic workup and treatment.
When symptomatic, small intestinal lipomas can cause a range of issues, primarily abdominal pain, which is often intermittent and non-specific [1]. Larger tumors may lead to complications such as intestinal obstruction, manifesting as abdominal cramping, nausea, vomiting, or intussusception, which can cause severe pain and bowel ischemia [1, 6, 7, 11, 27-29]. In rare cases, ulceration of the overlying mucosa can result in GI bleeding, evidenced by changes in stool appearance. Cheng [28] presented an interesting case of intermittent melena and abdominal colic due to small-bowel lipomatosis. The patient was found to have intussusception on imaging and the largest lipomas were resected using retrograde motorized spiral enteroscopy.
Symptomatic colorectal tumors can cause abdominal pain and bowel obstruction, presenting as abdominal bloating and changes in bowel habits or rectal discomfort, often confused with hemorrhoids [10, 12-14, 25, 26, 30]. In rare cases, erosion of a lipoma can result in significant bleeding, manifesting as bloody stools. Given their tendency to mimic malignancies, colorectal lipomas can predispose patients to significant perioperative morbidity and mortality [2, 3, 26]. Vishwajeet et al [3] reported the case of a 64-year-old male with a 1-month history of intermittent hematochezia and abdominal pain due to a giant pedunculated mass. Due to concern for colon cancer, the patient underwent laparoscopic left hemicolectomy, but the histopathology revealed a giant colonic lipoma.
| Diagnosis | ▴Top |
Computed tomography (CT) and magnetic resonance imaging (MRI) are essential diagnostic tools for identifying GI lipomas [12, 14]. On CT scans, lipomas appear as well-defined lesions with a characteristic fat density, typically measuring between -40 and -120 Hounsfield units, which aids in distinguishing them from denser GI tumors, such as GISTs or lymphomas [3, 4, 14, 26, 27]. MRI of the abdomen and pelvis enhances tissue characterization, particularly in complex cases, by displaying high signal intensity on T1-weighted and T2-weighted images, with lipomas losing signal on fat suppression sequences, confirming their fatty composition [4, 9, 17]. Both modalities provide detailed insights into the lipoma’s size, location, and any associated complications, such as obstruction.
Flexible or rigid endoscopy and colonoscopy offer direct visualization of GI lipomas, presenting them as smooth, rounded mucosal protrusions [13, 17]. During these procedures, lipomas may show the “tenting sign,” “naked fat sign,” “cushion sign,” or “pillow sign,” indicating their soft consistency, which is distinctive for such benign lesions [2-4, 15, 22, 26, 31]. Endoscopic ultrasound (EUS) further refines the diagnosis by determining the lesion’s layer of origin, typically the submucosa, and assessing its echogenicity, where lipomas appear homogeneous and hyperechoic [15]. EUS can also perform fine-needle aspirations or biopsies if the nature of the lesion remains uncertain, although this is rarely necessary for lipomas that exhibit typical imaging features [15, 25]. Together, these diagnostic techniques enable a thorough evaluation, aiding clinicians in differentiating benign lipomas from malignant neoplasms.
Because EUS image acquisition and interpretation are operator-dependent, tissue biopsy may be warranted in some cases for an accurate diagnosis [15, 25]. Histologically, lipomas appear as mature and well-differentiated adipocytes, with no mitotic figures or prominent fibrous septa [4, 6, 32]. Adipocytes typically appear uniform in size without nuclear hyperchromasia and cytologic atypia [15, 32]. On immunostaining, adipocytes stain positive for vimentin and S-100 and negative on MDM2 amplification studies [12, 24, 29, 32].
| Treatment and Outcomes | ▴Top |
Asymptomatic lipomas are managed conservatively with periodic imaging or endoscopy to assess for any changes in size or architecture. Symptomatic lipomas warrant endoscopic or surgical intervention to prevent further complications, such as ischemia and necrosis. Endoscopic techniques for accessible and medium-sized lipomas include endoscopic snare polypectomy, endoscopic mucosal resection (EMR), and endoscopic submucosal dissection (ESD) [3, 17, 28, 33-35]. These methods allow for precise removal of the lipoma while minimizing invasiveness and recovery time (Fig. 4). Deshmukh et al [18] performed a hybrid ESD of a giant esophageal lipoma in a male patient with dysphagia. The surgical defect was closed with endoclips and endoscopic suturing, and a relook endoscopy at 1 month showed a well-healed scar. Given the tortuosity of the small bowel, conventional EMR and ESD may have limited utility because of the higher risk of bleeding and perforation [1, 15]. Lipomas in the small intestine may require novel techniques such as double-balloon-assisted endoscopic resection or motorized spiral enteroscopy for effective sampling and resection [1, 7, 28]. Kobayashi et al [7] described a rare case of obscure GI bleeding due to jejunal lipoma that was resected endoscopically using the endoscopic unroofing technique. Although extremely rare, isolated cases of successful deployment of EMR or ESD in small bowel lipomas have been reported [33].
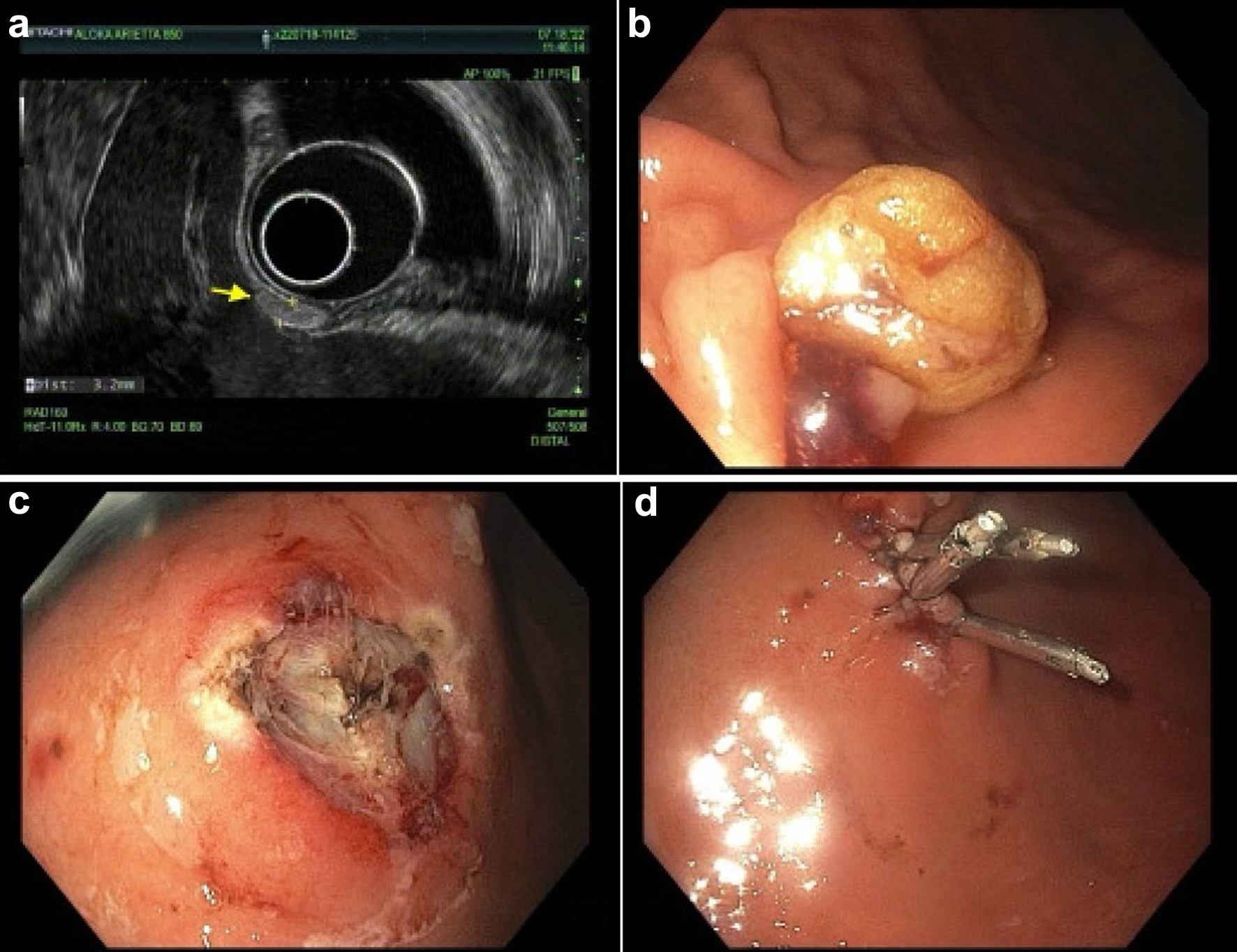 Click for large image | Figure 4. A library of endoscopy images showing the diagnosis and endoscopic mucosal resection of a gastric lipoma. (a) A hyperechoic oval nodule, measuring 3.2 mm in maximal cross-sectional diameter. There was sonographic evidence suggesting invasion into the submucosa. (b, c) A mucosectomy scar after mucosal resection of the lipoma. Three hemostatic clips were employed to close the surgical mucosal defect (d). |
In cases where lipomas are large, located in difficult-to-reach areas, or associated with severe symptoms such as significant obstruction, surgical intervention may be warranted [7, 10, 13, 14]. Surgical options include minimally invasive laparoscopic surgery, which offers the benefits of reduced recovery times and less post-operative pain, or traditional open surgery [14, 17, 29]. Emile et al [11] reported a unique case of small bowel volvulus due to a large mesenteric lipoma that required surgical exploration. Palacios et al [12] performed a right hemicolectomy with ileotransverse anastomosis in a patient with colo-colonic intussusception due to a lipoma at the hepatic flexure. The patient had an uneventful post-operative course and was discharged in stable condition. Rehal et al [5] shared an interesting case of a 52-year-old male who presented with a 2-month history of abdominal pain and heartburn due to a giant gastric lipoma. The patient underwent robotic wedge gastrectomy and complete resection of the 8 cm lipoma with no immediate complications. Post-intervention surveillance of GI lipomas is crucial to check for recurrence or complications. Although infrequent, surgical complications may occur, including luminal leakage, bleeding, infections, laceration of nearby visceral organs, and even death [1, 18].
| Conclusion | ▴Top |
Symptomatic GI lipomas present a unique clinical challenge due to their tendency to mimic other GI conditions, such as malignancy. Depending on their size and location, these benign tumors can cause dysphagia, abdominal pain, obstruction, or GI bleeding. Diagnosis primarily relies on imaging techniques, with CT and MRI providing clear tissue characterization and delineation from other submucosal lesions. Small, asymptomatic lipomas may simply require surveillance, whereas symptomatic lipomas often require intervention. Endoscopic techniques, such as snare polypectomy, EMR, and ESD, are preferred because of their minimally invasive nature and effectiveness. However, larger lipomas or those causing obstructions or intussusceptions often require surgical exploration. Post-operative follow-up is crucial for monitoring recurrence and managing any subsequent complications. This comprehensive review highlights the clinical presentation, diagnosis, and management of symptomatic GI lipomas.
Acknowledgments
None to declare.
Financial Disclosure
The authors declare that they do not have a financial relationship with any commercial entity that has an interest in the subject of this manuscript.
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Author Contributions
LB conceptualized the idea of this review article. HF, TW, DR, TR, and NS were involved in the literature review, data curation, and writing of the article. KA, YC, and WB edited and proofread the final draft prior to submission.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
Abbreviations
GI: gastrointestinal; GISTs: gastrointestinal stromal tumors; CT: computed tomography; MRI: magnetic resonance imaging; EUS: endoscopic ultrasound; EMR: endoscopic mucosal resection; ESD: endoscopic submucosal dissection
| References | ▴Top |
- Farkas N, Wong J, Bethel J, Monib S, Frampton A, Thomson S. A systematic review of symptomatic small bowel lipomas of the jejunum and ileum. Ann Med Surg (Lond). 2020;58:52-67.
doi pubmed pmc - Rezaii S, Enshaii A, Zahedi A, Amestejani M, Herik Dizaji M. Gastrointestinal bleeding due to gastrointestinal lipoma: A case report. Caspian J Intern Med. 2021;12(4):622-625.
doi pubmed pmc - Vishwajeet V, Soni S, Elhence P, Khera S. Giant lipoma of descending colon masquerading as a colonic malignancy. BMJ Case Rep. 2021;14(2):e237517.
doi pubmed pmc - Aqib A, Khan A, Venkata K. Giant Lipoma of Transverse Colon Presenting With Partial Obstruction of Intestine. Cureus. 2022;14(1):e21651.
doi pubmed pmc - Rehal M, Arya S, Anantha S, et al. S2504 Giant Gastric Cardia Lipoma. Am J Gastroenterol. 2022;117:e1667
- Brankovic B, Stanojevic G, Nestorovic M, Dencic T, Milutinovic N. Unusual cause of upper gastrointestinal bleeding. Report of the case of hemorrhagic duodenal lipoma with review of the literature. Ann Ital Chir. 2022;11:S2239253X22038014.
pubmed - Kobayashi R, Inoue K, Hirose R, Doi T, Harusato A, Dohi O, Yoshida N, et al. Obscure gastrointestinal bleeding from a large jejunal lipoma treated using an endoscopic unroofing technique with double balloon enteroscopy: a case study. Clin J Gastroenterol. 2023;16(1):32-38.
doi pubmed - Solano J, Herrera G, Cadena M, Cabrera LF, Isaac E, Pedraza M. Non surgical management for massive gastric lipomatosis. Int J Surg Case Rep. 2020;66:149-152.
doi pubmed pmc - Malla S, Razik A, Sharma R, Goyal A. Diffuse small bowel lipomatosis with intussusception. BMJ Case Rep. 2021;14(6):e242336.
doi pubmed pmc - Amirhom E, Dondapati M, Horton N, Pescovitz AR. Large colonic lipoma as a lead point for intussusception in an adult. J Surg Case Rep. 2022;2022(7):rjac327.
doi pubmed pmc - Emile SH, Sakr A, Sanad A. Small bowel volvulus secondary to mesenteric lipoma. J Gastrointest Surg. 2022;26(2):507-509.
doi pubmed - Palacios MF, Guachilema Ribadeneira A, Morocho Imbacuan S, Lisintuna Cisneros A, Basantes AD. Colonic lipoma of the hepatic flexure causing invagination in an adult. J Surg Case Rep. 2022;2022(9):rjac440.
doi pubmed pmc - Eshraghi Samani R, Salemi N, Firouzfar A. Colocolic intussusception because of lipoma in a 44-year-old adult. Adv Biomed Res. 2022;11:83.
doi pubmed pmc - Aassouani F, Bassim Alami G, Charifi Y, Assofi H, Attar A, El Bouardi N, Abid H, et al. Sigmoid lipoma as an exceptional cause of intussusception and bowel obstruction in adults: A case report and review of literature. Radiol Case Rep. 2022;17(10):3955-3958.
doi pubmed pmc - Sharzehi K, Sethi A, Savides T. AGA clinical practice update on management of subepithelial lesions encountered during routine endoscopy: expert review. Clin Gastroenterol Hepatol. 2022;20(11):2435-2443.e2434.
doi pubmed - Feldman J, Tejerina M, Hallowell M. Esophageal lipoma: a rare tumor. J Radiol Case Rep. 2012;6(7):17-22.
doi pubmed pmc - Ferrari D, Bernardi D, Siboni S, Lazzari V, Asti E, Bonavina L. Esophageal Lipoma and Liposarcoma: A Systematic Review. World J Surg. 2021;45(1):225-234.
doi pubmed pmc - Deshmukh A, Elmeligui A, Parsa N, Tejedor-Tejada J, Nieto J. Successful removal of a giant esophageal lipoma with hybrid endoscopic submucosal dissection. VideoGIE. 2021;6(9):398-400.
doi pubmed pmc - Bernardi D, Ferrari D, Siboni S, Porta M, Bruni B, Bonavina L. Minimally invasive approach to esophageal lipoma. J Surg Case Rep. 2020;2020(7):rjaa123.
doi pubmed pmc - Yekeler E, Yazicioglu A, Subasi M, Boztepe H. Giant Esophageal Lipoma as an Uncommon Cause of Diverticula. Case Rep Gastroenterol. 2016;10(2):446-451.
doi pubmed pmc - Yang B, Lu X. The malignancy among gastric submucosal tumor. Transl Cancer Res. 2019;8(7):2654-2666.
doi pubmed pmc - Cappell MS, Stevens CE, Amin M. Systematic review of giant gastric lipomas reported since 1980 and report of two new cases in a review of 117110 esophagogastroduodenoscopies. World J Gastroenterol. 2017;23(30):5619-5633.
doi pubmed pmc - Rahnemai-Azar AA, Rahnemaiazar AA, Naghshizadian R, Kurtz A, Farkas DT. Percutaneous endoscopic gastrostomy: indications, technique, complications and management. World J Gastroenterol. 2014;20(24):7739-7751.
doi pubmed pmc - Pintor-Tortolero J, Martinez-Nunez S, Tallon-Aguilar L, Padillo-Ruiz FJ. Colonic intussusception caused by giant lipoma: a rare cause of bowel obstruction. Int J Colorectal Dis. 2020;35(10):1973-1977.
doi pubmed - Anyfantakis D, Karona P, Kastanakis M. Rectal lipoma in an elderly male: a case report. Cureus. 2020;12(5):e8366.
doi pubmed pmc - Crocetti D, Sapienza P, Sterpetti AV, Paliotta A, A DEG, Pedulla G, de Toma G. Surgery for symptomatic colon lipoma: a systematic review of the literature. Anticancer Res. 2014;34(11):6271-6276.
pubmed - Bouali M, Sylvestre K, ElBakouri A, El Hattabi K, Bensardi FZ, Fadil A. Mesenteric lipoma with small bowel volvulus: A rare cause of upper gastrointestinal obstruction (a case report and literature review). Int J Surg Case Rep. 2022;92:106875.
doi pubmed pmc - Cheng K. Gastrointestinal: Successful management of lipomatosis in ileum by loop-and-let-go technique through motorized spiral enteroscopy. J Gastroenterol Hepatol. 2023;38(7):1017.
doi pubmed - Hu Q, Wu J, Sun Y. Intussusception related to small intestinal lipomas: a case report and review of the literature. Front Surg. 2022;9:915114.
doi pubmed pmc - Kang B, Zhang Q, Shang D, Ni Q, Muhammad F, Hou L, Cui W. Resolution of intussusception after spontaneous expulsion of an ileal lipoma per rectum: a case report and literature review. World J Surg Oncol. 2014;12:143.
doi pubmed pmc - Rodrigues DM, Parikh R, Maryala S, et al. Abstracts S127 24 Yo-Yo Lipoma in My Esophagus. http://journals.lww.com/ajg.
- Madhusudhan KS, Das P. Mesenchymal tumors of the stomach: radiologic and pathologic correlation. Abdom Radiol (NY). 2022;47(6):1988-2003.
doi pubmed - Noda H, Ogasawara N, Tamura Y, Kondo Y, Izawa S, Ebi M, Funaki Y, et al. Successful endoscopic submucosal dissection of a large terminal ileal lipoma. Case Rep Gastroenterol. 2016;10(3):506-511.
doi pubmed pmc - Orhan A, Demiryas S. Lipoma causing ileocecal intussusception and its endoscopic resection. Int J Surg Case Rep. 2022;98:107605.
doi pubmed pmc - Grande G, Pigo F, Caruso A, Russo S, Lupo M, Piccoli M, Conigliaro R. Too big to go out: gastric endoscopic submucosal dissection of giant lipoma complicated by intestinal obstruction. Endoscopy. 2021;53(12):E474-E475.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Current Surgery is published by Elmer Press Inc.